|
|
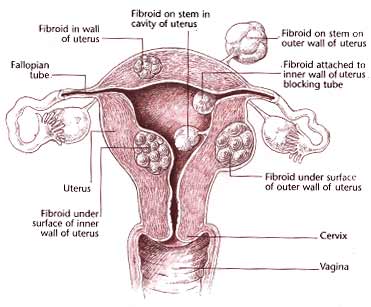
Fibroids (Fibromyomas)
Fibromyomas
(Fibroids or myomas) are benign neoplasms commonly encountered in
women in the reproductive age group. They are well circumscribed
tumours of smooth cells and interlacing fibrous tissues connective
cells.
Their growth is, in
or on the uterus. There might be some women who have no symptoms
with fibroids, other might experience pain or abnormal bleeding.
Fibroids may grow
on stems or remain a part of the uterus wall. They grow from the
muscle cell in the wall of the uterus as shown below.
The factors which
induce the growth of fibroids remains unidentified, but it is
suggested that contraction of the uterine muscles cause points of
stress within the myometrium (lining of uterus), which in turn
provides stimulus for the growth of immature cells inside and
outside the uterus.
Fibroids range from
the size of a pea to a size of a grapefruit. Estrogen, growth
hormone and human placental lactogen have been observed to promote
the development and growth of fibroids. For the same reason
fibroids have been observed to grow larger during pregnancy (when
estrogen productive increases) and shrink afterwards. Similarly as
women near menopause, their growth is halted, thus they shrink and
disappear.
Large number of
myomas (Fibroids) are encountered with no symptoms. The patient
may have first one symptom or may present with multiple symptoms,
depending on the size, number and location of tumours.
(a) (i) Menstrual
Disturbances:- Fibroids can cause an increase in the
amount, frequency or duration of menstrual bleeding due to
increased uterine surface, endometrial hyperplasia, and increased
uterine vascularity.
(ii)
Polymenorrhoea:- In some cases the menstrual bleeding might be
reduced with increase in the duration of haemorrhage.
(iii) Metrorrhagie:-
Intermenstrual bleeding occurs when the tumour is submucous and
protecting into the uterine cavity.
(b) Pain:-
Patient with large myomas might complain feeling of weight in the
pelvis or lower abdomen. Patient might complain of pain ranging
from mild to severe in abdomen or lower back.
(c) Pressure
Symptoms:- Fibroids situated in the posterior uterine wall or
situated in the pouch of Douglas may cause increase in the
frequency of urination or even, retention of urine in acute
stages.
(d) Infertility:-
Fibroids can cause infertility if they grow inside the uterus. A
fertilized egg may not be able to implant itself in the wall of
uterus. A fibroid that blocks the fallopian tube can cause
infertility by obstructing the passage of sperm or fertilized egg.
Large fibroids in the uterus can block the growth of a developing
fetus and cause premature labor.
Very rarely do
fibroids become cancerous. If they do occur, it is most often
after menopause. If a patient observes abdominal swelling,
painless in nature she must consult her doctor. A women suffering
from fibroids might be anaemic on account of menorrhagia.
Once the fibroids
have been identified, the doctor might intent to resort to some of
these measurers to examine the tumors more closely, using any one
these techniques:-
1. Ultrasound:-
It is useful in establishing the diagnosis of fibroids by creating
our image of the pelvic organ.
2. Laparoscopy:- Laparosope inserted
through a small incision just below the can enable the doctor to
view the interior of the pelvis. This might help the doctor to
rule out endometriosis, ectopic pregnancy and inversion prior to
laparotomy.
3. Hysteroscopy:- It enables the doctor to
insert a viewing instrument through the vagina and cervix to
examine the interior of the uterus.
4. A CAT scan helps to differentiate a myoma from
an adnexal mass.
5. Hysterosalpingography:- It is a method
of producing an X-ray image of the interior of the uterus and the
fallopian tubes to determine if there are any changes in the size
and shape of fibroids to check tubal blockage.
Treatment is not always necessary for fibroids
unless they cause excessive bleeding or pain or if the doctor is
not sure if the growth is a fibroid or a cancerous tumor.
In general, treatment may be conservative,
radiotherapeutic or operative.
CONSERVATIVE TREATMENT
1. Correction of Anaemia:- It us a course
of iron therapy is generally beneficial.
2. Danazol:- An androgenic and anti-oestrogenic,
given orally (400-800 mg in divided daily doses) for 3-6 months,
is seen to reduce the size of tumours.
3. Synthetic Gonadotropin:- Releasing
hormone (GnRH) analogue, administered either subcutaneously (200 mg
daily) or intranasally (300-400 mg three times daily) for six
months is reported to reduce the size of fibroids by 50-80%. This
treatment is useful in very young women and pre-menopausal women
as shrinkage of the tumour eliminates the need of surgery.
RADIOTHERAPY
This therapy is resorted to in very occasional
patients whose general condition is very poor and surgery needs to
be avoided. A women younger than 45 is not a suitable candidate
for radiotherapy. Besides patients on radiotherapy are liable to
develop uterine sarcoma at a later date.
OPERATIVE TREATMENT
The methods available are myomectomy, in which the
tumours are removed and the uterus is conserved and total
hysterectomy, when the uterus containing fibroids is removed.
(1) Myomectomy:- This is ideal for young
women who are anxious to have children or who are infertile and in
whom the infertility is attributed to fibroids. A woman in early
30s is best suited for myomectomy.
In the operation, the myometrium over the tumour
is incised and the tumour is completely shelled out from its
capsule. It can be a bloody operation and thus an adequate amount
of blood should be available during the operation.
(2) Hysterectomy:- Another treatment option
is hysterectomy or the removal of the uterus (and the fibroids
with it). This treatment is generally advised to women over 40 yrs
of age. Occasionally , hysterectomy may be indicated in young
women whose uterus is studded with fibroids, or if the tumours are
associated with bilateral tubo-ovarian masses.
Hormone treatment is usually given to women with
large fibroids to reduce the risk of bleeding during surgery, or
to shrink the fibroids enough to be able to hysterectomy through
the vagina instead through a incision in the abdomen.
REFERENCES :
-
Shawn's Book of Gynaecology ,Hawkins
& Bourne .eleventh edition
-
AMA ,A Complete Guide to Women's Health.
|
|
|
|
|









