|
|
Osteoporosis: Who are at Risk?
Osteoporosis
can be defined as a systemic skeletal disease characterised by low bone
mass and microarchitectural deterioration of bone tissue, with a consequent
increase in bone fragility and susceptibility to fracture.' Osteoporosis is
better preventable than treated.
 With its devastating
consequences including illness, pain functional limitations, reduced quality of
life, loss of independence, inability to work, and even death, Osteoporosis is a
serious disease. With its devastating
consequences including illness, pain functional limitations, reduced quality of
life, loss of independence, inability to work, and even death, Osteoporosis is a
serious disease.
Osteoporosis can
be classified into two main categories as follows:
1. Primary
Osteoporosis
a) Idiopathic : Occurs in
children and young adults where the cause is not known. Rare occurrence
b) Type I : Postmenopausal Osteoporosis- The cause of post menopausal osteoporosis is
unknown, however the 3 most significant contributing factors are believed to be:
-
Low levels of
estrogen, associated with menopause, are known to accelerate bone loss in
women.
-
Insufficient amounts
of calcium & vitamin D in the diet. Calcium is vital to the development
& maintenance of strong bones and vitamin D is required to absorb
calcium from the foods we eat.
-
Lack of physical
activity (common among many adults today) is believed to contribute to lower
bone density because the skeleton is not being taxed enough to stimulate
positive bone turn over
c) Type II : Senile Osteoporosis
2. Secondary
Osteoporosis
Osteoporosis resulting
from causes like chronic administration of drugs such as glucocorticoids,
diseases like Cushing's syndrome, surgical procedures including bilateral
oophorectomy, hystrectomy (removal of uterus). Kidney diseases and
some tumours
The
maintenance of bone mass depends upon the metabolic activity and turnover of the
skeleton, which in turn may affect the strength of bone by altering its
architecture. The adult skeleton is composed of two types of bone; cortical
(compact) which makes up 80% of the total bone mass and the trabecular
(cancellous) which constitutes about 20%. The cortical bone predominates the
skull and the shaft of the long bones. Trabecular bone on the other hand
is found in the vertebrae and the distal ends of the long bone.
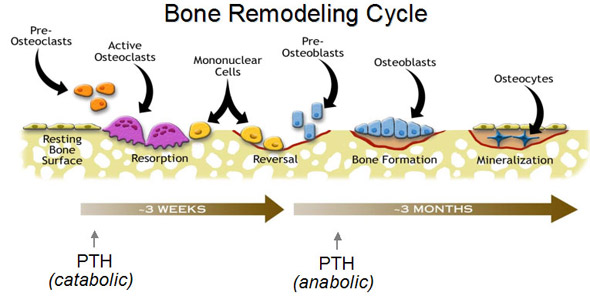
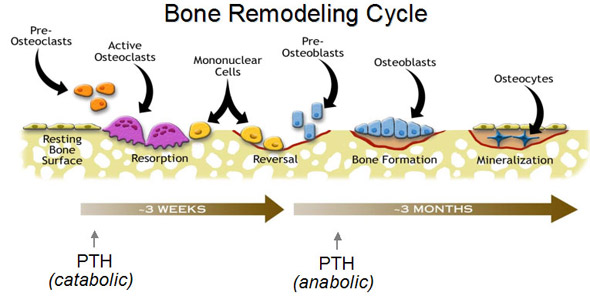
The process of removal of old
bone and replacement with repaired new bone is a continuous process in body.
this entire process is known as Bone turn over.
The whole skeletal bone turn over
occurs three times in life, first turn over is from birth to first year of life.
second is first year of life to skeletal maturity, and the third from adulthood
till rest of life. the procedure by which this turn over occurs is known as Bone
remodelling. The speed of remodelling would thus depend on the age and
physiological condition of the body.
In the healthy adult, bone mass
at skeletal maturity is neither increasing nor decreasing. There is considerable
turnover of bone, of which the majority (95%) is accounted for by bone
remodelling. Bone remodelling is a continuous complex process directed towards
renewal and repair of the skeleton and involves resorption followed by
formation. Since the bone turnover is dependent on the surface area it occurs
more rapidly in the trabecular bone than the cortical.
Normal Bone Mineral
Density
(gm/cm2) values in females |
Age |
Spine(L2-L4) |
Hip/Femoral
neck |
20
25
30
35 |
1.051
1.072
1.079
1.073 |
0.995
0.894
0.886
0.871 |
|
At the start of the remodelling
sequence, bone-resorbing cells (osteoclasts) migrate to or differentiate at a
specific location on the bone surface to dig a cavity. After this is
completed, the osteoclasts disappear; several days later, bone-forming cells
(osteoblasts) are attracted principally to sites of previous resorption and
infill the resorption cavity with new bone (Fig.2). The complete cycle takes
about six months. Normally, except in growing bones, the rates of bone
resorption and absorption are equal to each other so that the total bone mass
remains constant.
Osteoporotic
Bone Remodelling
The osteoporotic process may
involve a disorder in the remodelling process in which resorption exceeds
formation; either too much is being resorbed or too little is being formed.
A decrease in bone mass is caused by an imbalance between the amount of mineral
and matrix removed and subsequently incorporated into each resorption cavity, so
that skeletal mass decreases progressively. In postmenopausal and may other
types of Osteoporosis, the imbalance between the amount resorbed and that
formed at each remodelling site is caused by a decrease in the functional
capacity of osteoblasts recruited sites.
The absolute risk of developing
Osteoporosis depends on the individual's attainment of peak bone mass and
the rate and duration of bone loss thereafter. A decreased bone
mass is associated with increased risk of fracture. It has been shown that
the association between bone mass and fracture risk a stronger than that between
serum cholesterol and coronary events and that between systolic blood pressure
and stroke-associated mortality. Such fractures are known as Fragility
fractures.
Age
Peak bone mass is attained
between the ages of 25-35. Bone mass then begins to decline. Age-related
bone loss begins earlier and proceeds more rapidly in women, and there is a
trend towards acceleration of bone loss after menopauses averaging 2% per year
for the next 5 to 10 years followed by a slower rate of bone loss. Lifetime
losses may reach 30 to 40% of peak bone mass in women and 20 to 30% in men.
The risk factors for
Osteoporosis are as follows:
Individual Characteristics
-
Caucasian race or Asian
ethnicity
-
Menopause
-
Family history of
Osteoporosis
-
Low bone mass
-
Low body weight-
Small-boned and thin women (under 127 pounds) are at greater risk. (
compared to obese women who are protected due to conversion of some hormones
into anabolic hormones by the fat tissue).
-
Small stature
Lifestyle
-
Cigarette smoking
-
Alcohol abuse
-
Sedentary lifestyle
-
Inadequate calcium intake
-
Vitamin D deficiency
-
Excessive caffeine
-
Excessive exercise
Drug Use
-
Corticosteroids/glucocorticoids
-
Gonadotropin-releasing
hormones
-
Anticonvulsants
(Phenobarbital/phenytoin)
-
Heparin
For many
people, these are life-saving or life-enhancing drugs, and their use may be the
only way to achieve a better quality of life.
Secondary Causes
-
Cushing's syndrome
-
Anorexia nervosa
-
Mal absorption syndromes.
-
Hyperprolactinemia
-
Multiple myeloma
-
Hyperparathyroidism.
-
chromic Renal failures or
repeated dialysis
-
Rheumatoid Arthritis
-
Fragillitus oseum (in kids.)
-
Pagets disease.
Surgical Procedures
-
Bilateral oophorectomy
-
Gastrectomy
-
Hystrectomy
 Osteoporosis is a silent
disease in its initial stages and a careful interpretation of the clinical
evaluation is essential while diagnosing the disease. Clinical evaluation
should include both the history and the physical examination. The disease runs
long enough before symptoms appear, hence it should be looked for if there is a reason to suspect. Osteoporosis is a silent
disease in its initial stages and a careful interpretation of the clinical
evaluation is essential while diagnosing the disease. Clinical evaluation
should include both the history and the physical examination. The disease runs
long enough before symptoms appear, hence it should be looked for if there is a reason to suspect.
A postmenopausal woman, with
low back pain, a thin body frame, sedentary life style and a family history of
the disease is a sure candidate for Osteoporosis. The several risk
factors and the disease contributing to Osteoporosis should be taken into
consideration while evaluating a case of Osteoporosis.
Conventional X-ray is
relatively insensitive and bone loss is apparent only when the bone mass has
decreased by 30-50%. Bone biopsies also play a role in the study of
Osteoporosis. Recently, however, the advances in methods to diagnose
Osteoporosis and assess the risk of future fractures have been dramatic.
Non-invasive measurements of bone mineral density using bone densitometers
allow skeletal integrity, both centrally and peripherally, to be assessed with
an accuracy exceeding 95% and a precision doses.' The various bone densitometers
available are DEXA-Dual Energy X- ray Absorptiometry, pDEXA - peripheral DEXA,
SXA - Single X-ray Absorptiometry, RA - Radiographic Absorptiometry,
QCT-Quantitative Computer Tomography. Lately Ultrasonic bone densitometer
has been introduced which is safer than other densitometers since it does not
involve ionizing radiations, but has a lower accuracy.
A Bone Density Scan
Why you should do
it:
The early detection
of the risk of osteoporosis (a disease in which the bones become
fragile and more likely to break) can help determine the rate of bone
loss, predict your fracture risk in the future, and monitor the
effects of treatment over a period of time.
Normal bone
building takes place until the age of 35; thereafter the bone, as a
part of the natural ageing process, begins to break down faster than
new bone can be formed. Osteoporosis is preventable and can be
arrested at any stage. But if corrective action is not taken once
signs of the disease are detected, fractures can result more easily in
the hip, spine and wrist, requiring hospitalisation and may need
surgery. They are all pathology fractures that means the force
required to break the bone is far less than required for a normal
bone.
Hence beware it may
be just a turn in sleep to wake up with excruciating pain the fracture
of hip has perhaps resulted.
PROPHYLAXIS IS BETTER
THAN CURE. |
DEXA is still the 'Gold
Standard' for measuring bone density. The results of the densitometers are
interpreted in terms of T-scores. describes the bone mass of the patient
compared to the mean peak bone mass of the normal young adult reference
population using standard deviation.
The only Orthopaedic condition
recognised by W>H>O as public health hazard is Osteoporosis.
The World Health Organization
defines Osteoporosis using T-scores as follow:
Normal |
A
value of BMD that is within 1.0 SD of the young adult mean
|
Osteopenia |
A
value of BMD that is more than 1.0 SD blow the young adult mean but
less than 2.5 SD below this value |
Osteoporosis |
A
value of BMD that is 2.5 SD or more below the young adult mean
|
Severe Osteoporosis |
A
value of BMD that is more than 2.5 SD below the young adult mean in
the presence of one or more fragility fractures |
(BDM = Bone mineral density
SD = Standard deviation)
The rate of formation or
degradation of the bone matrix can be assessed either:
-
By measuring a
prominent enzymatic activity of the bone forming or resorbing cells such as
alkaline phosphatase etc.
-
By measuring bone matrix
components released into circulation during formation or resorption.
The use of sensitive
biochemical markers is gaining clinical importance. The potential uses of
biochemical markers are to assess the rate of bone turnover, to monitor
biochemical effects of therapy and to help evaluate patient compliance to
therapy. Pyridinoline and deoxypyridinoline cross-links are currently considered
'Gold Standard' in the assessment of bone resorption. In Osteoporosis, the
bone turnover is increased resulting in an increase in markers of bone formation
and bone resorption.
The following table shows the
biochemical markers used in current practice:
Formation
(Serum) |
Resorption
(Urine) |
Alkaline
phosphatase |
Hydroxyproline |
Osteocalcin |
Pyridinoline |
Procollagen I
extension
peptides |
Deoxypyridinoline |
Bone specific
alkaline Phosphatase |
N-telopeptide
crosslinks of type I collagen
|
The
dictum of medically healthy life is " IF YOU DO NOT USE IT YOU LOSE
IT" Hence use of bone needs pulling of structures attached on it i.e.
the muscles and tendons. so regular exercise grounds its importance. of bone needs pulling of structures attached on it i.e.
the muscles and tendons. so regular exercise grounds its importance.
Building strong
bones, especially before the age of 30, can be the best defense against
developing osteoporosis, and a healthy lifestyle can be critically important for
keeping bones strong.
-
Make exercise
or physical activity a part of your day-The
best exercise for your bones is weight-bearing exercise such as walking,
dancing, jogging, stair-climbing, racquet sports and hiking. If you have
been sedentary most of your adult life, be sure to check with your
healthcare provider before beginning any exercise program.
Tips for
trouble-Free Exercise
-
Lift
and lower weight slowly to maxirnize muscle strength and minimize the
risk
of injury.
-
It's
best to perform your resistance workout every third day. This gives your
body a chance to recover.
-
Avoid
exercise the puts excessive stress on your bones, such as running or
high-impact aerobics. Avoid rowing machines-they require deep forward
bending that may lead to a vertebral fracture.
-
Stiffness
in the morning after exercise is normal. But if you're in pain most of
the following day, your joints are swollen, or you're limping stop the
program until your joints are swollen, or and cut your weights and
repetitions by 25% to 50% If bone, joint, or muscle pain is severe, cell
your doctor.
-
If a
particular area of your body feels sore right after exercise, apply ice
for 10 to 15 minutes. Wrap ice in a towel or baggie, or just hold a cold
can of soda to the spot.
-
Vary
your routing to make it more interesting. For example, if your
strength-building program involves 12 separate exercises, do six in one
session and the other six in the next.
|
-
 Bones react
to load by gradually growing stronger & denser. Bones react
to load by gradually growing stronger & denser.
Recent
studies have
shown that the risk of osteoporosis is lower for people who are
active, and especially those who do load-bearing, or weight-bearing
activities at least three times a week. The best exercises are
weight-lifting, jogging, hiking, stair-climbing, step aerobics, dancing,
racquet sports, and other activities that require your muscles to work
against gravity. Swimming and simply walking, although good for
cardiovascular fitness, are not the best exercises for building bone. Thirty
minutes of weight-bearing exercise daily benefits not only your bones, but
improves heart health, muscle strength, coordination, and balance. Those 30
minutes don't need to be done all at once; it's just as good for you to do
10 minutes at a time. Log on to
http://ag.arizona.edu/maricopa/fcs/bb/bbchart.htm,
to check out the bone building exercise chart for beginners, intermediate
and advanced trainers.
Put
LIVE into action!
| |
|
|
L |
- |
Load or
weight-bearing exercises make a difference to your bones. |
I |
- |
Intensity builds
stronger bones. |
V |
- |
Vary the types of
exercise and your routine to keep interested. |
E |
- |
Enjoy your
exercises. Make exercise fun so you will continue into the future! |
|
-
Quit
smoking and reduce your risk for osteoporosis & most other
diseases.
-
Reduce
soft drink consumption. The phosphorus in soft drinks appears to
have a deleterious effect on bone tissue. Colas & beverages with
caffeine & phosphorus appear to cause bone resorption (problem for
children & adults).
-
Alcohol consumption under control
-
Be sure to get your daily
dose of calcium and vitamin D, both nutrients are necessary to
build & maintain bone tissue. The recommended does for postmenopausal
women below 65 years of age is 1000 mg/day and 1500 mg/day above 65 years of
age. Vitamin D is needed for the body to absorb
calcium. Without enough vitamin D, you will be unable to absorb calcium from
the foods you eat, and your body will have to take calcium from your bones.
Vitamin D comes from two sources: through the skin following direct exposure
to sunlight and from the diet. Experts recommend a daily intake between 400
and 800 IU per day, which also can be obtained from fortified dairy
products, egg yolks, saltwater fish and liver.
For sources of calcium in diet
click
here.
-
See your doctor for a Bone
Mineral Density Test, after age 50. A Bone Mineral
Density test (BMD) is the only way to diagnose osteoporosis and determine
your risk for future fracture. Since osteoporosis can develop undetected for
decades until a fracture occurs, early diagnosis is important.
Drugs
used in the treatment of Osteoporosis:
Drugs used in the treatment and
prevention of Osteoporosis are traditionally classified as antiresorptive and
anabolic. The majority of those currently licensed, fall into the former
category. The predominant effect of antiresorptive agents is
to prevent bone loss, although small increases in bone mass may occur.
Hormone replacement therapy, calcitonin and bisphosphonates are the major
antiresorptive drugs used. Anabolic drugs like Anabolic steroids on
the other hand have the potential to increase bone mass.
Sodium flouride in high doses
spoils the bones but in small doses it acts as bone hardener. It also has an
anabolic action. Its medical use is debatable. Calcitonin now can be given as
nasal spray (MIACALCIC) Parathyroid hormone also is
anabolic in small doses.
HRT:
Estrogen is believed to
act directly on bone cells through high affinity estrogen receptors expressed by
osteoblasts. Though the exact mechanism is still not known, estrogen is believed
to inhibit bone resorption. HRT and estrogen replacement therapy (ERT) have been
approved by the FDA for the prevention and, for some products, management of
osteoporosis. There are side effects of oestrogens. see below.
However the research is now
directed to find chemical compounds which would have action like that of
oestrogen but, they would act only on bones etc. they are known as S.E.R.M.
Raloxifene
(Brand name: Evista�) is a selective estrogen receptor modulator (SERM)approved by the FDA for both prevention and treatment of osteoporosis in
postmenopausal women.
However, HRT has several
contraindications e.g.. breast or endometrial tumors, uncontrolled hypertension,
chronic or acute hepatic diseases, recent thromboembolic, cardiovascular or
coronary artery disease, endometriosis, uterine myelomas, etc. Short
term adverse effects of hormone replacement therapy include vaginal bleeding,
breast tenderness and upper gastrointestinal symptoms.
Calcitonin
Calcitonin primarily inhibits
bone resportion by inhibiting osteoclast function as well as by reducing
osteoclast number. It is FDA-approved for the
treatment of osteoporosis in women who are at least 5 years postmenopausal. It
is delivered as a single daily intranasal spray and subcutaneous administration
by injection also is available.
Bisphosphonates
Bisphosphonates are synthetic,
non-biodegradable analogues of pyrophosphate which inhibit bone resorption.
Etidronate is the first generation bisphosphonate used to treat Osteoporosis.
Its propensity to inhibit mineralization however limits its use and
necessitates its cyclic administration.
Alendronate is a third
generation bisphosphonate and the first non-hormonal therapy approved by the
U.S. FDA for the treatment and prevention of Osteoporosis. In vivo
studies indicate that Alendronate is 1000 times more potent than etidronate.
Various clinical trials have
shown that daily treatment with Alendronate 10 mg progressively increases
bone mass in the spine, hip, and total body and reduce the incidence of
vertebral and nonvertebral fractures and height loss in postmenopausal women
with Osteoporosis. The low incidence of side effects and good
tolerability of Alendronate is also evident from these studies. Thus Alendronate
fulfills the ultimate goal of Osteoporosis management which is the reduction in
the incidence of fractures. Alendronate is now available in single weekly doses. Its
effect appears in some months, Hence the drug should as a rule be started the day
menopausal symptoms start knocking the door.
Pamidronate the new compound is
under trial and may prove more promising.
I. Premenopause
A. Eumenorrheic
-
Physiological calcium (700 to 1300 mg/day)
-
Vitamin D (400
international units/day)
-
Exercise
B.
Amenorrheic
-
physiological calcium (700 to 1300 mg/day)
-
Consider cyclical estrogen and progestin*
-
Vitamin D (400
international units/day)
-
Appropriate caloric intake
-
Exercise
II. Postmenopause
A. Bone mineral density
within 1 standard deviation less than that of peers
-
Calcium
(1500 mg/day)
-
Vitamin D (400 international units/day)
-
Consider cyclical estrogen and progestin if patient* <70 yrs. old
B.
Bone mineral density 1 to 2.5 standard deviations less than of peers and no
fracture
-
Calcium (1500 mg/day)
-
Vitamin
D (400 international units/day)
-
Cyclical estrogen and
progestin* if patient <70 yrs. old
C. Bone mineral density
>2.5 standard deviations less than of peers. or fracture
-
Calcium (1500 mg/day)
-
Vitamin D (400 international units/day)
-
Calcitonin (50 to 100 units subcutaneously. 3 to 7 days/wk.) acutely. for as long as 18 mos.
-
Then, cyclical estrogen and progestin* if
patient <70 yrs. old, or alendronate (10.0 mg/day) if bone mineral density
>2.5 standard deviations less than that peers, as food and Drug
Administration recommendations.
|
Although much remains to be
learned about the causes and management of Osteoporosis, the
constant research in this field is giving clinicians a wider range of
therapeutic options. Women interested in bone health,
whether or not they are postmenopausal, should practice bone-healthy behaviors.
It is important to get the daily-recommended dosage of calcium and vitamin D;
engage in regular weight-bearing exercise; avoid smoking and excessive alcohol.
Most important of all: women need to know their own family-health history and
discuss treatment options regularly with their health care professional.
Related Links
|
|
|
|
|
 of bone needs pulling of structures attached on it i.e.
the muscles and tendons. so regular exercise grounds its importance.
of bone needs pulling of structures attached on it i.e.
the muscles and tendons. so regular exercise grounds its importance. Bones react
to load by gradually growing stronger & denser.
Bones react
to load by gradually growing stronger & denser.





 Osteoporosis is a silent
disease in its initial stages and a careful interpretation of the clinical
evaluation is essential while diagnosing the disease. Clinical evaluation
should include both the history and the physical examination. The disease runs
long enough before symptoms appear, hence it should be looked for if there is a reason to suspect.
Osteoporosis is a silent
disease in its initial stages and a careful interpretation of the clinical
evaluation is essential while diagnosing the disease. Clinical evaluation
should include both the history and the physical examination. The disease runs
long enough before symptoms appear, hence it should be looked for if there is a reason to suspect.