Retinitis Pigmentosa
How to use a Mask
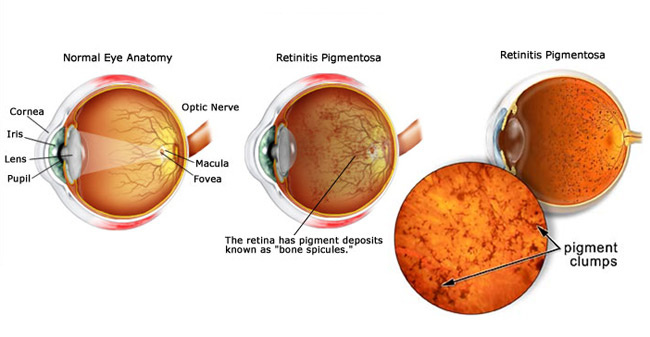
An inherited progressive degeneration in the retina, the light - sensitive
membrane at the back of the eye. Speaking, generically it can be described as a
progressive cause of visual loss, which is attributed to the loss of viable
photoreceptors.
In humans there are two types of light sensitive cells in the retina: rod cells
and cone cells. Rod cells
pick
up movement out of the corner of the eye and also, in a normal eye it is the
rods that operate in poor light or at night. There are about 120 million rods in
each eye and they are more numerous towards the outer edge of the retina. The
cone cells are used in colour vision and in close precision work like reading.
There are not as many cones and they are more concentrated in the centre of the
retina (the Macula).
Retinitis pigmentosa is a rare disorder in which the cells in the light -
sensitive retina in the eye are progressively lost. Dark patches of pigment form
on the retina, and vision deteriorates. The disorder is more common in males and
is inherited, usually in an autosomal recessive manner. It may not cause
symptoms until early in adult life. Both eyes are affected equally.
Causes
Retinitis
Pigmentosa can be inherited from our parents as genes carry family traits like
eye and hair color, the shape of our face, etc. Retinitis Pigmentosa can be
passed to succeeding generations by one of three genetic inheritance patterns-autosomal
dominant, autosomal recessive, or X-linked inheritance.
RP may be caused by a breakdown in the function of the rods or the cones in some
part of the retina. The retina is so complex that breakdowns may occur in a
variety of ways and so RP is not a single disorder but a great number of
disorders. The breakdown of cone function may be called
Macular Degeneration.
There are other disorders similar to RP like Gyrate Atrophy, Choroideremia etc.
The common feature is the degeneration of the retina for one reason or another.
Researchers are trying to find particular causes of retinal disorders.

Symptoms
If you have retinitis pigmentosa, the first symptom you may notice is poor vision in dim light. Later, the outer edges of vision, known as peripheral vision, are lost, and sight deteriorates progressively inwards until only a small area of central vision remains. Rarely, tunnel vision can cause blindness
-
Difficulty in seeing at night or in poor illumination. Most forms of RP first
cause the degeneration of rod cells. These forms of Retinitis pigmentosa,
sometimes called rod-cone dystrophy, usually begin with night blindness.
-
Glare.
-
Eye fatigue (from straining to see).
-
Low light to dark adaptation times and poor contrast sensitivity.
- Other forms of Retinitis Pigmentosa, sometimes called cone-rod dystrophy, first affect central vision. Patients first experience a loss of central vision that cannot be corrected with glasses or contact lenses.
Diagnosis
Retinitis pigmentosa is diagnosed by
examining the retina with an
ophthalmoscope, an instrument which directs a beam of light into the eye. The
classic sign of RP is clumps of pigment in the peripheral retinal called "bone-spicules."
A test called electroretinography (ERG) may also be ordered to study the eye's
response to light stimuli. The test gives the health care provider information
about the function of the rods and cones in the retina.

Treatment
There is no effective treatment or cure for retinitis pigmentosa (RP). Treatment
aims to decrease further vision loss and to help you function with the vision
that you have. Your doctor can counsel you about expected patterns of vision
loss based on the type of retinitis pigmentosa you have.
Although the condition is untreatable, special
glasses may help to widen the
field of vision if your visual loss becomes severe. Also, the use of sunglasses
to protect the retina from ultraviolet light may have a vision-preserving
effect.
Bionic Eye Implant: Opening Doors for Visually Impaired
Bionic Vision Australia researchers have successfully performed the first
bionic eye implant of an early prototype at the Royal Victorian Eye and Ear Hospital in
Melbourne. The bionic eye was implanted in a woman who has profound vision loss
due to retinitis pigmentosa, an inherited condition.
Feedback from Ms Ashworth (the patient) will allow researchers to develop a
vision processor so that images can be built using flashes of light. This early
prototype does not incorporate an external camera - yet. This is planned for the
next stage of development and testing. The team at Royal Victorian Eye and Ear
Hospital in Melbourne is looking for consistency of shapes, brightness, size and
location of flashes to determine how the brain interprets this information.
Having this unique information will allow us to maximise our technology as it
evolves through 2013 and 2014
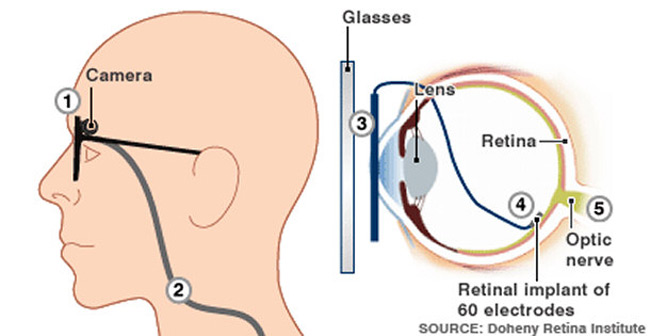
image source: http://news.bbc.co.uk/
What the process involves?
The Argus II system uses a to feed visual information to electrodes in the eye.
A spectacle-mounted camera is used to capture real-time images, and a processing unit, about the size of a small handheld computer and worn on a belt, converts the visual information into electrical signals. These are then sent back to the glasses and wirelessly on to a receiver just under the surface of the front of the eye, which in turn feeds them to the electrodes at the rear. The whole process happens in real time.
This can be a ray of hope for about 1.5 million people worldwide having retinitis pigmentosa, and one in 10 people over the age of 55 having age-related macular degeneration.
Supplement
For people with Retinitis Pigmentosa a daily dose of 15000 International units
of Vitamin A Palmitate (only) has been shown to slow the degeneration of the
cone ERG. A blood test must be taken to ascertain liver function and Vitamin A
levels in the blood BEFORE taking this treatment. Pregnant women must not take
high doses of Vitamin A under any circumstances and this treatment must be
undertaken in consultation with your doctor or eye specialist.
These include the following:
-
Magnifying glasses
-
Electronic magnifiers, which project an enlarged image onto a screen
-
Night vision scopes, which enlarge distant objects under conditions of low light
- Lenses for distant vision (eyeglasses or contacts)
If you plan to have children, you may wish to have genetic counseling to assess
the risk of the abnormal gene being inherited.
