|
|
|
 , ,
Font size |
Top 10 Worst and Dangerous Incurable Diseases in the world
 Small Cell Lung Cancer Small Cell Lung Cancer
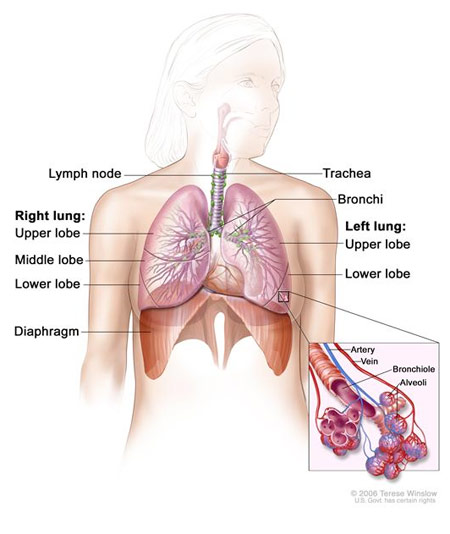
Lung
cancer is a deadly disease in which the average survival is 2 to 4 months
without treatment, says MedlinePlus. It states that 15 percent of lung cancers
are of the small cell type. This type of lung cancer can rapidly spread and
create havoc in the body.
Symptoms of small cell lung cancer include shortness of breath, wheezing,
coughing up blood, unintentional weight loss and chest pain. This type of lung
cancer can also lead to a poor appetite, fever, hoarseness, difficulty
swallowing and facial swelling. In some cases, it can lead to weakness and
changes in the voice. Small cell lung cancer typically occurs as a result of
smoking.
Chemotherapy medications such as etopside, along with radiation treatment may
help manage the symptoms of small cell lung cancer but does not cure it.
MedlinePlus says that surgery only helps a few people as small cell lung cancer
typically spreads by the time it is discovered.
Small-cell carcinoma (sometimes known as "small-cell lung cancer", or "oat-cell
carcinoma") is a type of highly malignant cancer that most commonly arises
within the lung, although it can occasionally arise in other body sites, such as
the cervix, prostate, and gastrointesinal tract.
Small-cell carcinoma is an undifferentiated neoplasm composed of
primitive-appearing cells.
As the name implies, the cells in small-cell carcinomas are smaller than normal
cells, and barely have room for any cytoplasm. Some researchers identify this as
a failure in the mechanism that controls the size of the cells.
In a significant number of cases, small-cell carcinomas can produce ectopic
hormones, including adrenocorticotropic hormone (ACTH) and anti-diuretic hormone
(ADH). Ectopic production of large amounts of ADH leads to syndrome of
inappropriate antidiuretic hormone hypersecretion (SIADH). Lambert-Eaton
myasthenic syndrome (LEMS) is a well-known paraneoplastic condition linked to
small-cell carcinoma.
Histopathologic image of small-cell carcinoma of the lung. CT-guided core needle
biopsy. H&E stain. When associated with the lung, it is sometimes called "oat
cell carcinoma" due to the flat cell shape and scanty cytoplasm. It is thought
to originate from neuroendocrine cells (APUD cells) in the bronchus called
Feyrter cells (named for Friedrich Feyrter). Hence, they express a variety of
neuroendocrine markers, and may lead to ectopic production of hormones like ADH
and ACTH that may result in paraneoplastic syndromes and Cushing's syndrome.
Approximately half of all individuals diagnosed with Lambert-Eaton myasthenic
syndrome (LEMS) will eventually be found to have a small-cell carcinoma of the
lung.
Small-cell carcinoma is most often more rapidly and widely metastatic than
non-small cell lung carcinoma (and hence staged differently). There is usually
early involvement of the hilar and mediastinal lymph nodes.
Combined small-cell lung carcinoma (c-SCLC)
Small-cell lung carcinoma can occur in combination with a wide variety of other
histological variants of lung cancer, including extremely complex malignant
tissue admixtures. When it is found with one or more differentiated forms of
lung cancer, such as squamous cell carcinoma or adenocarcinoma, the malignant
tumor is then diagnosed and classified as a combined small cell lung carcinoma
(c-SCLC). C-SCLC is the only currently recognized subtype of SCLC. Although
combined small-cell lung carcinoma is currently staged and treated similarly to
"pure" small-cell carcinoma of the lung, recent research suggests surgery might
improve outcomes in very early stages of this tumor type.
Smoking is a significant etiological factor.
Symptoms and signs are as for other lung cancers. In addition, because of their
neuroendocrine cell origin, small-cell carcinomas will often secrete substances
that result in paraneoplastic syndromes such as Lambert-Eaton myasthenic
syndrome.
Extrapulmonary small-cell carcinoma
Very rarely, the primary site for small-cell carcinoma is outside of the lungs
and pleural space, it is referred to as extrapulmonary small-cell carcinoma (EPSCC).
Outside of the respiratory tract, small cell carcinoma can appear in the cervix,
prostate, liver, pancreas, gastrointestinal tract, or bladder. It is estimated
to account for 1,000 new cases a year in the U.S. Histologically similar to
small-cell lung cancer, therapies for small-cell lung cancer are usually used to
treat EPSCC. First line treatment is usually with cisplatin and etoposide. In
Japan, the first line treatment is shifting to irinotecan and cisplatin. When
the primary site is in the skin, it is referred to as Merkel cell carcinoma.
Small-cell carcinoma of the prostate
 In the prostate, small-cell carcinoma (SCCP) is a rare form of cancer (approx 1%
of PC). Due to the fact that there is little variation in prostate specific
antigen levels, this form of cancer is normally diagnosed at an advanced stage,
after metastasis. It can metastasize to the brain. In the prostate, small-cell carcinoma (SCCP) is a rare form of cancer (approx 1%
of PC). Due to the fact that there is little variation in prostate specific
antigen levels, this form of cancer is normally diagnosed at an advanced stage,
after metastasis. It can metastasize to the brain.
Small-cell lung carcinoma has long been divided into two clinicopathological
stages, including limited stage (LS) and extensive stage (ES). The stage is
generally determined by the presence or absence of metastases, whether or not
the tumor appears limited to the thorax, and whether or not the entire tumor
burden within the chest can feasibly be encompassed within a single radiotherapy
portal. In general, if the tumor is confined to one lung and the lymph nodes
close to that lung, the cancer is said to be LS. If the cancer has spread beyond
that, it is said to be ES.
In cases of LS-SCLC, combination chemotherapy (often including cyclophosphamide,
cisplatinum, doxorubicin, etoposide, vincristine and/or paclitaxel) is
administered together with concurrent chest radiotherapy (RT). Chest RT has been
shown to improve survival in LS-SCLC.
Exceptionally high objective initial response rates (RR) of between 60% and 90%
are seen in LS-SCLC using chemotherapy alone, with between 45% and 75% of
individuals showing a "complete response" (CR), which is defined as the
disappearance of all radiological and clinical signs of tumor. Unfortunately,
relapse is the rule, and median survival is only 18 to 24 months.
Because SCLC usually metastasizes widely very early on in the natural history of
the tumor, and because nearly all cases respond dramatically to CT and/or RT,
there has been little role for surgery in this disease since the 1970s. However,
recent work suggests that in cases of small, asymptomatic, node-negative SCLC's
("very limited stage"), surgical excision may improve survival when used prior
to chemotherapy.("adjuvant chemotherapy").
In ES-SCLC, combination chemotherapy is the standard of care, with radiotherapy
added only to palliate symptoms such as dyspnea, pain from liver or bone
metastases, or for treatment of brain metastases, which, in small-cell lung
carcinoma, typically have a rapid, if temporary, response to whole brain
radiotherapy.
Combination chemotherapy consists of a wide variety of agents, including
cisplatin, cyclophosphamide, vincristine and carboplatin. Response rates are
high even in extensive disease, with between 15% and 30% of subjects having a
complete response to combination chemotherapy, and the vast majority having at
least some objective response. Responses in ES-SCLC are often of short duration,
however.
If complete response to chemotherapy occurs in a subject with SCLC, then
prophylactic cranial irradiation (PCI) is often used in an attempt to prevent
the emergence of brain metastases. Although this treatment is often effective,
it can cause hair loss and fatigue. Prospective randomized trials with almost
two years follow-up have not shown neurocognitive ill-effects. Meta-analyses of
randomized trials confirm that PCI provides significant survival benefits. All
in all, small-cell carcinoma is very responsive to chemotherapy and
radiotherapy, and in particular, regimens based on platinum-containing agents.
However, most people with the disease relapse, and median survival remains low.
In limited-stage disease, median survival with treatment is 14�20 months, and
about 20% of patients with limited-stage small-cell lung carcinoma live 5 years
or longer. Because of its predisposition for early metastasis, the prognosis of
SCLC is poor with only 10% to 15% of patients surviving 3 years (Washington and
Leaver, 2010).
The prognosis is far worse in extensive-stage small-cell lung carcinoma, with
treatment, median survival is just 8�13 months, and only 1�5% of patients with
extensive-stage small-cell lung carcinoma treated with chemotherapy live 5 years
or longer.
Next..
Dated 19 October 2013
|
|
|
|
|
|
|









