|
|
High-Risk Pregnancy: Oligohydramnios
Too much or too little amniotic
fluid
 Amniotic
fluid is an important part of pregnancy
and fetal development. This watery fluid
is inside a casing called the amniotic
membrane (or sac) and fluid surrounds
the fetus throughout pregnancy. Normal
amounts may vary, but, generally, women
carry about 500 ml of amniotic fluid.
Amniotic fluid helps protect and cushion
the fetus and plays an important role in
the development of many of the fetal
organs including the lungs, kidneys, and
gastrointestinal tract. Fluid is
produced by the fetal lungs and kidneys.
It is taken up with fetal swallowing and
sent across the placenta to the mother's
circulation. Amniotic fluid problems
occur in about 7 percent of pregnancies. Amniotic
fluid is an important part of pregnancy
and fetal development. This watery fluid
is inside a casing called the amniotic
membrane (or sac) and fluid surrounds
the fetus throughout pregnancy. Normal
amounts may vary, but, generally, women
carry about 500 ml of amniotic fluid.
Amniotic fluid helps protect and cushion
the fetus and plays an important role in
the development of many of the fetal
organs including the lungs, kidneys, and
gastrointestinal tract. Fluid is
produced by the fetal lungs and kidneys.
It is taken up with fetal swallowing and
sent across the placenta to the mother's
circulation. Amniotic fluid problems
occur in about 7 percent of pregnancies.
Hydramnios (too much amniotic fluid)
poses a greater threat to the mother,
whereas Oligohydramnios (too little of
amniotic fluid) poses greater danger to
the life of the fetus that she is
carrying.
The Amniotic Fluid Index
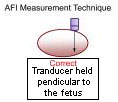
 How
is the level of amniotic fluid measured?
Your health care provider uses
ultrasound to measure the depth of the
amniotic fluid in four different areas
of your uterus and adds up the results.
This is your amniotic fluid index. If
the amniotic fluid depth is less than 5
centimeters (cm), you have
oligohydramnios. If the depth measures
greater than 25 cm, you have
polyhydramnios. How
is the level of amniotic fluid measured?
Your health care provider uses
ultrasound to measure the depth of the
amniotic fluid in four different areas
of your uterus and adds up the results.
This is your amniotic fluid index. If
the amniotic fluid depth is less than 5
centimeters (cm), you have
oligohydramnios. If the depth measures
greater than 25 cm, you have
polyhydramnios.
Oligohydramnios
 Oligohydramnios
is a condition in which there is too
little amniotic fluid around the fetus.
The condition is often the result of a
tear or rupture in the amniotic
membrane, causing it to leak amniotic
fluid and thus lower the level of fluid
still surrounding the baby It occurs in
about 4 percent of all pregnancies. Oligohydramnios
is a condition in which there is too
little amniotic fluid around the fetus.
The condition is often the result of a
tear or rupture in the amniotic
membrane, causing it to leak amniotic
fluid and thus lower the level of fluid
still surrounding the baby It occurs in
about 4 percent of all pregnancies.
What causes oligohydramnios?
There are several causes of
oligohydramnios. Generally, it is caused
by conditions that prevent or reduce
amniotic fluid production. Factors that
are associated with oligohydramnios
include the following:
-
Premature rupture of membranes
(before labor)
-
Intrauterine growth restriction
(poor fetal growth)
-
Post-term pregnancy
-
Birth defects, especially kidney
and urinary tract malformations. If
his kidneys aren't developing
properly (Potter's syndrome) or his
urinary tract is blocked, your baby
won't be able to produce enough
urine to keep the level of amniotic
fluid up.
-
 Twin-to-twin
transfusion syndrome - This happens
when there's a problem with the
placenta and one twin ends up with a
disproportionate share of the blood
supply. The "donor" twin suffers
from low amniotic fluid, while the
"recipient" twin usually ends up
with too much. About two-thirds of
twins with this syndrome don't
survive the pregnancy. Twin-to-twin
transfusion syndrome - This happens
when there's a problem with the
placenta and one twin ends up with a
disproportionate share of the blood
supply. The "donor" twin suffers
from low amniotic fluid, while the
"recipient" twin usually ends up
with too much. About two-thirds of
twins with this syndrome don't
survive the pregnancy.
-
 Certain
drugs may cause oligohydramnios,
including ACE inhibitors, which are
often used for management of high
blood pressure, and prostaglandin
inhibitors, such as indomethacin or
even ibuprofen. You should avoid
these drugs during pregnancy Certain
drugs may cause oligohydramnios,
including ACE inhibitors, which are
often used for management of high
blood pressure, and prostaglandin
inhibitors, such as indomethacin or
even ibuprofen. You should avoid
these drugs during pregnancy
Amniotic fluid is
important in the development
of fetal organs, especially
the lungs. Too little fluid
for long periods may cause
abnormal or incomplete
development of the lungs
called pulmonary hypoplasia.
Intrauterine growth
restriction (poor fetal
growth) is also associated
with decreased amounts of
amniotic fluid.
Oligohydramnios may be a
complication at delivery,
increasing the risk for
compression of the umbilical
cord and aspiration of thick
meconium (baby's first bowel
movement).
|
What are the symptoms of
oligohydramnios?
The following are the most common
symptoms of oligohydramnios. However,
each woman may experience symptoms
differently. Symptoms may include:
-
Leaking of amniotic fluid when
the cause is rupture of the amniotic
sac
-
Decreased amount of amniotic
fluid on ultrasound
The symptoms of the oligohydramnios may
resemble other medical conditions.
Always consult your physician for a
diagnosis.
Diagnosis
 In
addition to a complete medical history
and physical examination, a
diagnosis is usually made using
ultrasound. Pockets of amniotic
fluid can be measured and the total
amount estimated. If it is between two
and five centimeters, this is considered
low Ultrasound can also show fetal
growth, the structure of the kidneys and
urinary tract, and detect urine in the
fetal bladder. Doppler flow studies may
be used to check the arteries in the
kidneys. In
addition to a complete medical history
and physical examination, a
diagnosis is usually made using
ultrasound. Pockets of amniotic
fluid can be measured and the total
amount estimated. If it is between two
and five centimeters, this is considered
low Ultrasound can also show fetal
growth, the structure of the kidneys and
urinary tract, and detect urine in the
fetal bladder. Doppler flow studies may
be used to check the arteries in the
kidneys.
Treatment for oligohydramnios:
Specific treatment for oligohydramnios
will be determined by your physician
based on:
-
Your pregnancy, overall health,
and medical history
-
Extent of the condition
-
Your tolerance for specific
medications, procedures, or
therapies
-
Expectations for the course of
the condition
-
Your opinion or preference
Treatment for oligohydramnios may
include:
-
Closely monitoring the amount of
amniotic fluid and frequent
follow-up visits with the physician
-
 Amnioinfusion Amnioinfusion
-
instilling a special fluid into the
amniotic sac to replace lost or low
levels of amniotic fluid.
Amnioinfusion is still experimental,
but it may be offered during
pregnancy in an attempt to help
prevent pulmonary hypoplasia
(underdeveloped lungs), or at
delivery to help prevent compression
of the umbilical cord.
-
Delivery. Often, this means
weighing the risks of inducing labor
versus leaving the baby in-utero
until it reaches greater maturity
According to the
American Journal of
Obstetrics, pregnant women
who find themselves
diagnosed with
oligohydramnios should pay
particular attention to
eating a balanced diet and
receiving regular prenatal
care
|
Complications list for
Oligohydramnios:
The list of complications that have been
mentioned in various sources for
Oligohydramnios includes:
Prevention
In order to prevent polyhydramnios or
oligohydramnios, it would be necessary
to prevent the underlying cause. Good
control of maternal diabetes and the
prevention of infections transmittable
from mother to fetus are two approaches
for a subset of cases, but, in general,
prevention is not possible.
HIGH
RISK PREGNANCY : HYDRAMNIOS
Dated 20 January 2009
Related Links
|
|
|
|
|





 Amniotic
fluid is an important part of pregnancy
and fetal development. This watery fluid
is inside a casing called the amniotic
membrane (or sac) and fluid surrounds
the fetus throughout pregnancy. Normal
amounts may vary, but, generally, women
carry about 500 ml of amniotic fluid.
Amniotic fluid helps protect and cushion
the fetus and plays an important role in
the development of many of the fetal
organs including the lungs, kidneys, and
gastrointestinal tract. Fluid is
produced by the fetal lungs and kidneys.
It is taken up with fetal swallowing and
sent across the placenta to the mother's
circulation. Amniotic fluid problems
occur in about 7 percent of pregnancies.
Amniotic
fluid is an important part of pregnancy
and fetal development. This watery fluid
is inside a casing called the amniotic
membrane (or sac) and fluid surrounds
the fetus throughout pregnancy. Normal
amounts may vary, but, generally, women
carry about 500 ml of amniotic fluid.
Amniotic fluid helps protect and cushion
the fetus and plays an important role in
the development of many of the fetal
organs including the lungs, kidneys, and
gastrointestinal tract. Fluid is
produced by the fetal lungs and kidneys.
It is taken up with fetal swallowing and
sent across the placenta to the mother's
circulation. Amniotic fluid problems
occur in about 7 percent of pregnancies.
 How
is the level of amniotic fluid measured?
Your health care provider uses
ultrasound to measure the depth of the
amniotic fluid in four different areas
of your uterus and adds up the results.
This is your amniotic fluid index. If
the amniotic fluid depth is less than 5
centimeters (cm), you have
oligohydramnios. If the depth measures
greater than 25 cm, you have
polyhydramnios.
How
is the level of amniotic fluid measured?
Your health care provider uses
ultrasound to measure the depth of the
amniotic fluid in four different areas
of your uterus and adds up the results.
This is your amniotic fluid index. If
the amniotic fluid depth is less than 5
centimeters (cm), you have
oligohydramnios. If the depth measures
greater than 25 cm, you have
polyhydramnios. Oligohydramnios
is a condition in which there is too
little amniotic fluid around the fetus.
The condition is often the result of a
tear or rupture in the amniotic
membrane, causing it to leak amniotic
fluid and thus lower the level of fluid
still surrounding the baby It occurs in
about 4 percent of all pregnancies.
Oligohydramnios
is a condition in which there is too
little amniotic fluid around the fetus.
The condition is often the result of a
tear or rupture in the amniotic
membrane, causing it to leak amniotic
fluid and thus lower the level of fluid
still surrounding the baby It occurs in
about 4 percent of all pregnancies.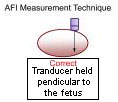
 Twin-to-twin
transfusion syndrome - This happens
when there's a problem with the
placenta and one twin ends up with a
disproportionate share of the blood
supply. The "donor" twin suffers
from low amniotic fluid, while the
"recipient" twin usually ends up
with too much. About two-thirds of
twins with this syndrome don't
survive the pregnancy.
Twin-to-twin
transfusion syndrome - This happens
when there's a problem with the
placenta and one twin ends up with a
disproportionate share of the blood
supply. The "donor" twin suffers
from low amniotic fluid, while the
"recipient" twin usually ends up
with too much. About two-thirds of
twins with this syndrome don't
survive the pregnancy. Certain
drugs may cause oligohydramnios,
including ACE inhibitors, which are
often used for management of high
blood pressure, and prostaglandin
inhibitors, such as indomethacin or
even ibuprofen. You should avoid
these drugs during pregnancy
Certain
drugs may cause oligohydramnios,
including ACE inhibitors, which are
often used for management of high
blood pressure, and prostaglandin
inhibitors, such as indomethacin or
even ibuprofen. You should avoid
these drugs during pregnancy In
addition to a complete medical history
and physical examination, a
In
addition to a complete medical history
and physical examination, a
 Amnioinfusion
Amnioinfusion