New Menopausal Symptom Management Guidelines 2014

The American College of Obstetricians and Gynecologists (ACOG) updated its
evidence-based guidelines for the treatment of vasomotor and vaginal symptoms
associated with natural and surgical menopause.
The updated bulletin, replaces the June 2001 version and was published in the
January 2014 issue of Obstetrics & Gynecology.
Vasomotor Symptoms of Menopause
The decline in concentrations of gonadal hormones during
menopause gives rise to a range of physiologic and psychologic changes that may
impact a woman's health and quality of life significantly. Symptoms including night
sweats and hot
flashes occur in 85% of
perimenopausal women. They start 1-2 years before Menopause and continue for up
to 5 years.
Vaginal Symptoms
Less estrogen may cause the tissues of the vulva and the lining of the vagina to
become thinner, drier, and less elastic or flexible. Shifting levels of
hormones—especially estrogen—during the menopause transition produce changes in
a woman’s body. Both the vagina and the external female genitals (vulva) are
affected leading to Vulvovaginal atrophy ( lining of the vagina to become
thinner, drier, and less elastic or flexible) and Atrophic
vaginitis (inflamation of vagina).
| Vaginal lining with estrogen |
Vaginal lining in low-estrogen state |
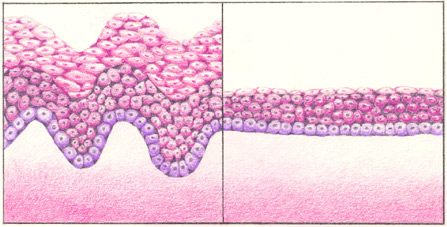
Lining of the vagina before menopause (left) and after menopause (right).
Before menopause, when the vagina is well supplied with estrogen, its lining
is thicker and has more folds, allowing it to stretch with intercourse and
childbirth. After menopause, when levels of estrogen are low, the vaginal
lining is thinner and has fewer folds, which makes it less flexible.
New Recommendations for Menopausal Symptom Management are
listed in 3 tiers:
Level A ("good or consistent scientific evidence"):
-
Systemic HT, with just estrogen or estrogen plus
progestin, is the most effective approach for treating vasomotor symptoms.
-
Low-dose and ultra-low systemic doses of estrogen have a more favorable
adverse effect profile than standard doses.
-
Healthcare providers should individualize care and use the lowest
effective dose for the shortest duration.
-
Thromboembolic disease and breast cancer are risks associated with use
of combined systemic HT.
-
SSRIs (selective serotonin reuptake inhibitors), SSNRIs (selective
serotonin and norepinephrine reuptake inhibitors), clonidine, and gabapentin
relieve vasomotor symptoms and are alternatives to HT.
-
Local estrogen therapy is advised for isolated atrophic vaginal
symptoms.
-
The only non-hormonal therapy approved to treat vasomotor symptoms is
paroxetine, and ospemifene is approved to treat dyspareunia.
Level B conclusions ("limited or inconsistent scientific evidence"):
-
 Data do not support use of progestin alone, testosterone, compounded
bioidentical hormones, phytoestrogens, herbal supplements,
and lifestyle modifications. Data do not support use of progestin alone, testosterone, compounded
bioidentical hormones, phytoestrogens, herbal supplements,
and lifestyle modifications.
-
"Common sense lifestyle solutions" are layering clothing, lowering room
temperature, and consuming cool drinks.
-
Nonestrogen water-based or silicone-based lubricants and
moisturizers may alleviate pain.
Level C recommendation ("based primarily on consensus and expert opinion"):
-
Individualize the decision to continue HT. The new Practice Bulletin
states that HT should not be discontinued at age 65 years, because some
women have hot flushes longer.
The report mentions FDA approval of 2 new drugs: bazedoxifene instead of
progestin with conjugated estrogen for hot flushes and osteoporosis prevention,
and ospemifene for vaginal dryness that may cause dyspareunia.
Note: Because all medications have potential side effects and risks associated
with their use, it is important to weigh the potential risks and benefits of
treatment.
Ref:
http://www.medscape.org/
Dated 21 January 2014
Related Links
|









