Colorectal Cancer cancer of the colon or rectum
The colon and the rectum are part of the large
intestine, which is part of the digestive system. Because colon cancer and
rectal cancers have many features in common, they are sometimes referred to
together as colorectal cancer. Colorectal cancer includes cancers of both the
large intestine (colon), the lower part of your digestive system, and the
rectum, the last 8 to 10 inches of the colon.
Most colon and rectal cancers begin as small,
noncancerous (benign) clumps of cells called adenomatous polyps. Over time some
of these polyps become cancerous.
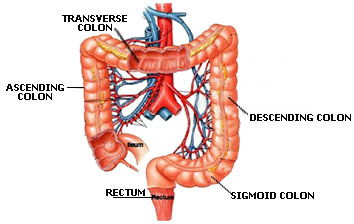
The colon is the first 6 feet of the large intestine. It has four sections:
-
The first section is called the ascending colon. It extends upward on the right
side of the abdomen.
-
The second section is called the transverse colon since it goes across the body
to the left side.
-
There it joins the third section, the descending colon, which continues downward
on the left side.
-
The fourth section is known as the sigmoid colon because of its S-shape. The
sigmoid colon joins the rectum, which, in turn, joins the anus, or the opening
where waste matter passes out of the body.
There are several causes for colorectal cancer as well as factors that place
certain individuals at increased risk for the disease. There are known genetic
and environmental factors.
People at risk for colorectal cancer:
-
The biggest risk factor is age.
Colorectal cancer is rare in those under 40 years. The rate of colorectal
cancer detection begins to increase after age 40. Most colorectal cancer is
diagnosed in those over 60 years.
-
Have a mother, father, sister,
or brother who developed colorectal cancer or polyps. When more than one
family member has had colorectal cancer, the risk to other members may be
three-to-four times higher of developing
the
disease. This higher risk may be due to an inherited gene.
-
Have history of benign
growths, such as polyps, that have been surgically removed.
-
Have a prior history of
colon or rectal cancer.
-
Have disease or condition linked
with increased risk.
-
Have a diet high in
fat and low in
fiber.
Having certain diseases or conditions may place
people at increas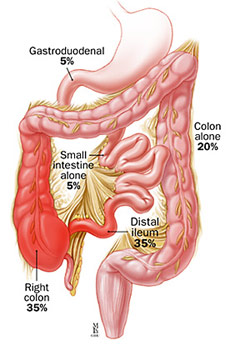 ed
risk for colorectal cancer. These include ed
risk for colorectal cancer. These include
-
Chronic
ulcerative colitis, an inflammatory condition of the colon. People in this
risk category have long-term disease, most for ten years or more.
-
Crohn's
disease,
which is an inflammatory disease of the gastrointestinal
tract. This disease may increase colorectal cancer risk, although not as much
ulcerative colitis.
-
-
Inherited a specific colorectal
cancer syndrome. Those with an inherited syndromes may develop colorectal
cancer at a much younger age, in their 30s or even younger. Over the past
several years, genetic forms of colorectal cancer have been identified and
genetic tests developed.
Symptoms of
colorectal cancer
The symptoms of colorectal cancer can be confused
with those of a number of digestive disorders. Having one or more of these
symptoms does not mean you have cancer
The following are the most common symptoms of
colorectal cancer. However, each individual may experience symptoms differently.
Women who have any of the following symptoms
should check with their physicians, especially if they are over 40 years old or
have a personal or family history of the disease:
-
A change in bowel habits such as
diarrhea, constipation, or
narrowing of the stool that lasts for more than a few days.
-
Rectal bleeding or blood in the
stool
-
Cramping or gnawing stomach pain
-
Decreased appetite
-
Vomiting
-
Unexplained weight loss,
unusually low red blood cell counts or
anemia, weakness and
fatigue
-
Jaundice (yellowish coloring) of
the skin or sclera of the eye
The symptoms of colorectal cancer may resemble
other conditions, such as infections,
hemorrhoids, and
inflammatory bowel disease. It is also possible to have colon cancer and not
have any symptoms. Always consult your physician for a diagnosis.
Most colon cancers develop from polyps. Screening is extremely important for
detecting polyps before they become cancerous. It can also help find colorectal
cancer in its early stages when you have a good chance for recovery.
The doctor performs a thorough clinical evaluation
that includes:
-
A complete medical, family, and
drug history
-
A physical examination,
including a digital rectal examination
Common screening and diagnostic
procedures include the following:
-
Digital rectal exam. In this office exam, your doctor uses a gloved finger to
check the first few inches of your rectum for large polyps and cancers.
Although safe and painless, the exam is limited to your lower rectum and can't
detect problems with your upper rectum and colon. In addition, it's difficult
for your doctor to feel small polyps.
-
 Fecal occult (hidden) blood test. This test checks a
sample of your stool for blood. It can be performed in your doctor's office,
but you're usually given a kit that explains how to take the sample at home.
You then return the sample to a lab or your doctor's office to be checked. The
problem is that not all cancers bleed, and those that do often bleed
intermittently. Furthermore, most polyps don't bleed. This can result in a
negative test result, even though you may have cancer. On the other hand, if
blood shows up in your stool, it may be the result of hemorrhoids or an
intestinal condition other than cancer. For these reasons, many doctors
recommend other screening methods instead of, or in addition to, fecal occult
blood tests. Fecal occult (hidden) blood test. This test checks a
sample of your stool for blood. It can be performed in your doctor's office,
but you're usually given a kit that explains how to take the sample at home.
You then return the sample to a lab or your doctor's office to be checked. The
problem is that not all cancers bleed, and those that do often bleed
intermittently. Furthermore, most polyps don't bleed. This can result in a
negative test result, even though you may have cancer. On the other hand, if
blood shows up in your stool, it may be the result of hemorrhoids or an
intestinal condition other than cancer. For these reasons, many doctors
recommend other screening methods instead of, or in addition to, fecal occult
blood tests.
-
Flexible sigmoidoscopy.
In this test, your doctor uses a
flexible, slender and lighted tube to examine your rectum and sigmoid
approximately the last 2 feet of your colon. Nearly half of all colon cancers
occur in this area. The test usually takes just a few minutes. It can
sometimes be somewhat uncomfortable, and there's a slight risk of perforating
the colon wall.
-
Barium enema. This diagnostic test allows your doctor to
evaluate your entire large intestine with an X-ray. Barium, a contrast dye, is
placed into your bowel in an enema form. During a double contrast barium
enema, air is also added. The barium fills and coats the lining of the bowel,
creating a clear silhouette of your rectum, colon and sometimes a small
portion of your small intestine. This test typically takes about 20 minutes
and can be somewhat uncomfortable. There's also a slight risk of perforating
the colon wall. A flexible sigmoidoscopy is often done in addition to the
barium enema to aid in detecting small polyps that a barium enema X-ray may
miss, especially in the lower bowel and rectum.
-
Colonoscopy.
This procedure is the most sensitive test for
colorectal cancer and polyps. Colonoscopy is similar to flexible sigmoidoscopy,
but the instrument used a colonoscope, which is a long, flexible and slender
tube attached to a video camera and monitor allows your doctor to view your
entire colon and rectum. If any polyps are found during the exam, your doctor
may remove them immediately or take tissue samples (biopsies) for analysis.
This is done through the colonoscope and is painless. If you have adenomatous
polyps, especially those larger than 5 millimeters in diameter, you'll need
careful screening in the future.
A colonoscopy takes about a half-hour. You may
receive a mild sedative to make you more comfortable. Preparation for the
procedure involves drinking a large amount of fluid containing a laxative to
clean out your colon enemas are no longer necessary. Major risks of
diagnostic colonoscopy include hemorrhage and perforation of the colon wall.
But these risks are rare. Complications may be somewhat more frequent when
polyps are removed.
-
Genetic testing. If you have a family history of colorectal cancer, you
may be a candidate for genetic testing. This blood test may help determine if
you're at increased risk of colon or rectal cancer, but it's not without
drawbacks. The results can be ambiguous, and the presence of a defective gene
doesn't necessarily mean you'll develop cancer. Knowing you have a genetic
predisposition can alert you to the need for regular screening. Still, you'll
also want to consider the psychological impact of what the test may reveal.
Knowing you may develop cancer affects not only your own life, but the lives
of everyone close to you. Genetic testing for children is even more complex
and problematic. It's best if you discuss all of the ramifications of genetic
testing with your doctor or a medical geneticist.
Another new test checks a stool sample for DNA
from abnormal cells. In preliminary studies, the test has proved to be so
accurate it may eventually eliminate the need for more-invasive examinations
such as colonoscopy, at least in average-risk circumstances. A three-year
clinical trial of this test by the National Cancer Institute is under way.
Screening Guidelines for Colorectal Cancer
Colorectal cancer screening guidelines
from the American Cancer Society for early detection include:
-
Beginning at age 50,
both men and women should follow this testing schedule: Digital rectal
examination should be performed at the time of each screening
sigmoidoscopy, colonoscopy, or barium enema examination.
-
Yearly fecal occult
blood test, plus:
-
flexible sigmoidoscopy
every 5 years, or
-
colonoscopy every 10
years, or
-
double contrast barium
enema every 5-10 years
-
People with any of the
following colorectal cancer risk factors should begin screening
procedures at an earlier age:
-
strong family history of
colorectal cancer or polyps (cancer or polyps in a first degree
relative younger than 60 or in two first degree relatives of any age)
-
family with hereditary
colorectal cancer syndromes (familial adenomatous polyposis and
hereditary non-polyposis colon cancer)
-
personal history of
colorectal cancer or adenomatous polyps
-
|
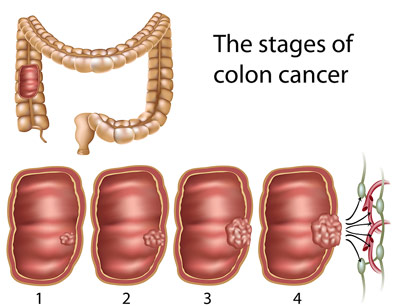
Staging of
Colorectal Cancer
Staging is the process of finding out how far the cancer has spread. This is
very important because your treatment and the outlook for your recovery depend
on the stage of your cancer. For early cancer, surgery may be all that is
needed. For more advanced cancer, other treatments such as chemotherapy or
radiation therapy may be used.
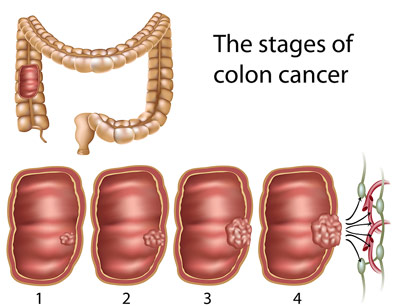
Stage 0
For cancers that are stage 0, the disease has
not grown beyond the lining of the colon or rectum. Therefore surgical removal
or destruction of the cancer is all that is needed. For larger tumors, a rectal
or colon resection may be required.
Stage 1
For
colon cancer, Stage 1 cancers have grown through several layers of the colon but
have not spread outside the colon itself. Standard treatment is a colon
resection with no other treatment generally needed.
Like colon cancer, Stage 1 rectal cancers have
grown through numerous layers of tissue but not outside the rectum. The type of
surgery used to treat this is dependant upon the location of the cancer, but the
primary treatment is an abdominoperineal resection. Chemotherapy and radiation
are sometimes administered before or after surgery.
Stage 2
Stage 2 colon cancer has penetrated the wall
of the colon and spread into nearby tissue. However, it has not yet reached the
lymph nodes. Usually the only treatment for this stage is a resection. Since
some Stage 2 colon cancers have a tendency to recur, the doctor may also decide
to treat the patient with chemotherapy or radiation therapy.
Once rectal cancer has reached Stage 2, it too has
penetrated the walls of the rectum but has not yet reached the lymph nodes. It
is generally treated with a resection and then both chemotherapy and radiation
therapy.
Stage 3
Stage 3 is considered an advanced stage of
colorectal cancer. The disease has spread to the lymph nodes, but not to other
parts or organs in the body. For both colon and rectal cancer, sectional surgery
is done first and is followed by chemotherapy and radiation therapy.
Stage 4
For patients with Stage 4 colorectal cancer,
the disease has spread to distant organs such as the liver, lungs and ovaries.
When the cancer has reached this stage, surgery is generally aimed at relieving
or preventing complications as opposed to curing the patient of the disease.
Occasionally the cancers spread is restricted enough to where it can all be
removed by surgery. For Stage 4 cancer that cannot be surgically removed,
chemotherapy, radiation therapy or both may be used to alleviate, delay or
prevent symptoms
Treatment
for colorectal cancer
Specific treatment for colorectal cancer will be
determined by your physician based on:
-
your age, overall health, and
medical history
-
extent of
the disease
-
your tolerance for specific
medications, procedures, or therapies
-
expectations for the course of
the disease
-
your opinion or preference
Treatment choices for the person with colon cancer
depend on the stage of the tumor - if it has spread and how far. When the
disease has been found and staged, your physician will suggest a treatment plan.
Treatment may include:
-
Colon surgery
Often, the primary treatment for colorectal cancer is an
operation called a segmental resection, in which the cancer and a length of
normal tissue on either side of the cancer are removed, as well as the nearby
lymph nodes.
-
Radiation therapy
Radiation therapy is the use of high-energy radiation to
kill cancer cells either after surgery, to kill small areas of cancer that may
not be seen during surgery, or instead of surgery. Radiation may also be used
to ease (palliate) symptoms such as pain, bleeding, or blockage. There are two
ways to deliver radiation therapy, including the following:
-
External beam
radiation
External beam radiation uses radiation from
outside the body, which is focused on the cancer.
-
Internal
radiation therapy
Internal radiation therapy uses small pellets of
radioactive material placed directly into the cancer.
-
Chemotherapy
Drugs (medications) are given into a vein or by
mouth to kill
cancer cells throughout the body. Studies have shown that chemotherapy after
surgery can increase the survival rate for patients with some stages of colon
cancer. Chemotherapy can also help relieve symptoms of advanced cancer.
Dated 14th March, 2005
Related Links
|





 ed
risk for colorectal cancer. These include
ed
risk for colorectal cancer. These include  Fecal occult (hidden) blood test. This test checks a
sample of your stool for blood. It can be performed in your doctor's office,
but you're usually given a kit that explains how to take the sample at home.
You then return the sample to a lab or your doctor's office to be checked. The
problem is that not all cancers bleed, and those that do often bleed
intermittently. Furthermore, most polyps don't bleed. This can result in a
negative test result, even though you may have cancer. On the other hand, if
blood shows up in your stool, it may be the result of hemorrhoids or an
intestinal condition other than cancer. For these reasons, many doctors
recommend other screening methods instead of, or in addition to, fecal occult
blood tests.
Fecal occult (hidden) blood test. This test checks a
sample of your stool for blood. It can be performed in your doctor's office,
but you're usually given a kit that explains how to take the sample at home.
You then return the sample to a lab or your doctor's office to be checked. The
problem is that not all cancers bleed, and those that do often bleed
intermittently. Furthermore, most polyps don't bleed. This can result in a
negative test result, even though you may have cancer. On the other hand, if
blood shows up in your stool, it may be the result of hemorrhoids or an
intestinal condition other than cancer. For these reasons, many doctors
recommend other screening methods instead of, or in addition to, fecal occult
blood tests.