|
 , ,
Font size |
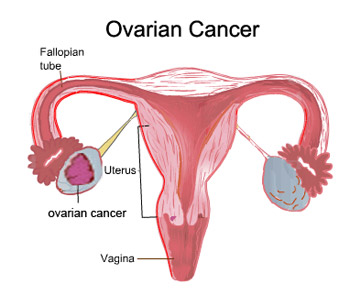
Ovarian Cancer
Ovarian cancer is the second most common
reproductive cancer in women after endometrial cancer. Cancer
occurs when cells
undergo a transformation and begin to grow and multiply without normal controls.
As the cells grow and multiply, they form masses called tumors. Ovarian cancer
occurs when a tumor forms in one or both of a woman's ovaries.
Ovarian tumors are classified on the basis of the type of cell from which the
abnormal growth originated.
-
Epithelial tumors: These tumors arise from a layer of cells that surrounds
the outside of the ovary called the germinal epithelium. About 70-80% of all
ovarian cancers are epithelial. These are usually found in women who have been
through menopause (aged 45-70 years).
-
Stromal tumors: Stromal tumors develop from connective tissue cells that
help form the structure of the ovary and produce hormones. Usually, only one
ovary is involved. These account for 5-10% of ovarian cancers. These tumors
typically occur in women aged 40-60 years. Often, surgical removal of the
tumor is the only treatment needed. If the tumor has spread, though,
chemotherapy is needed.
-
Germ cell tumors: Tumors that arise from germ cells (cells that produce
the egg) account for about 15% of all ovarian cancers. These tumors develop
most often in young women (including teenaged girls). Although 90% of women
with this type of cancer are successfully treated, many become permanently
infertile.
-
Metastatic tumors: Only 5% of ovarian cancers have spread from other
sites. The most common sites from which they spread are the colon (52%),
breast (17%), stomach (10%), and pancreas (5%).
-
Within these main classes are many different subtypes of tumors.
Ovarian Cancer is much more likely to be
fatal than cancer of the cervix or endometrium because it is more difficult to
detect at an early stage.
Stages of ovarian cancer
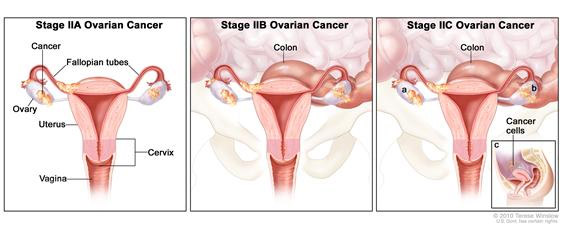
Ovarian Cancer is also identified by a series of i>stages. The stage
describes the extent of the disease at the time of
diagnosis, including tumor
size and whether the cancer has spread (metastasized) to other areas of the
body. The stages are commonly described as follows:
Stage I - Growth of tumor limited to the ovaries
Stage II - Growth of tumor in one or both ovaries
Stage III - Tumor involving one or both ovaries with peritoneal implants
outside the pelvis and/or positive retroperitoneal or inguinal lymph nodes.
Superficial liver metastasis equals stage III.
Stage IV - Growth involving one or both ovaries with distant metastases. If
pleural effusion is present there must be positive cytology to allot a case to
stage IV. Tumor spread inside the liver, equals stage IV.
Recurrent/Refractory - Recurrence means that the tumor has returned after
initial therapy. Refractory means that the tumor fails to respond to initial
treatment.
What are the common symptoms?
Symptoms Ovarian caner has no symptoms in the early stages. The
cancer is most often detected when a doctor feels an enlarged ovary during a
routine pelvic examination or while he or she is investigating
other problems in the reproductive tract. At more advanced stages, a woman
with ovarian cancer may have vague intestinal problems, a sensation of fullness,
and abdominal or pelvic pain or discomfort. (As the cancer
progress, it causes fluid to build up inside the abdomen.) Often a woman's
first indication of a problem is noticing that her waistline is expanding for no
apparent reasons and her clothes don't fit. Occasionally, bleeding, like
a period, may occur in a woman who has passed the
menopause. At this stage, a
woman may become
anaemic, may lose her appetite, may lose weight and may start
to feel unusually tired.
If the cancer spreads to places outside the abdomen, other symptoms may
develop. For example, if the liver is involved, then the skin and the whites of
the eyes may turn yellow: this is called jaundice. If the lungs are affected,
then this may cause breathlessness and coughing. Ovarian cancer is a fatal
condition if it is not treated.
What causes ovarian cancer and who is at risk?
Regular ovulation that is not interrupted by pregnancy or
breast-feeding appears to play a major role in the development of ovarian
cancer. In the process of ovulation, cells in the ovaries are continuously
dividing. The constant cellular activity increases the possibility of
genetic mistakes occurring in ovarian cells, which can lead to cancer.
Ovarian cancer has been linked with 3 hereditary
syndromes.
-
Breast-ovarian cancer syndrome
-
Hereditary nonpolyposis colorectal cancer syndrome
-
Site-specific ovarian cancer syndrome
|
The following factors increase a
woman's risk of ovarian cancer:
-
Never having children- Term
pregnancy (lasting the full 9 months) significantly reduces the risk of
ovarian cancer. As the number of pregnancies increases, the risk of ovarian
cancer decreases. Besides, Breastfeeding lowers risk of ovarian cancer, and
the risk decreases with increasing duration of breastfeeding.
-
Having children at an older age
-
Going through menopause late
(after age 55)
-
 High-Fat Diet - Ovarian Cancer
has been linked to an increased amount of estrogen activity in the body.
Excess fat can cause the body to retain estrogen and may convert other
hormones into a form of estrogen, increasing the risks of Ovarian Cancer. High-Fat Diet - Ovarian Cancer
has been linked to an increased amount of estrogen activity in the body.
Excess fat can cause the body to retain estrogen and may convert other
hormones into a form of estrogen, increasing the risks of Ovarian Cancer.
-
Never having taken oral
contraceptives (which block ovulation) Some studies have shown that the
use of fertility drugs
increases the risk of ovarian cancer, but study results have not been
consistent.
-
Having family history of cancer
of the colon, breast, prostate, or lung
-
Having a history of cancer of
the breast, endometrium, or colon and rectum. There is a known inheritable
genetic mutation that puts women at a higher risk for developing Ovarian
Cancer. If a woman has one or more primary relatives (mother or sister) who
have had Ovarian Cancer, she is three times more likely to be diagnosed with
the disease herself. Genetic testing can be done on women in this "high risk"
group to determine if they carry one of the gene mutations. Being a carrier of
this gene does not necessarily mean that a woman has or will develop Ovarian
Cancer. It simply means that a woman is at a higher risk of developing Ovarian
Cancer and should be followed very closely for evidence of the disease.
-
Being white- White women are
much more likely to have ovarian cancer than African American women.
Diagnosis
 There is no uniformly accepted test for Ovarian Cancer at this time. The
ovaries are difficult to examine since they are set deep in the abdomen.
Annual pelvic and rectal examinations in which the doctor feels for any
abnormalities in the ovaries are the best ways to detect early signs of ovarian
cancer in women with no symptoms or known risk factors. Another way to
determine if a woman has Ovarian Cancer is to take a sample of ovary and
abdominal tissue (Biopsy). The tissue sample is then examined under a
microscope to determine if cancer cells are present. There is no uniformly accepted test for Ovarian Cancer at this time. The
ovaries are difficult to examine since they are set deep in the abdomen.
Annual pelvic and rectal examinations in which the doctor feels for any
abnormalities in the ovaries are the best ways to detect early signs of ovarian
cancer in women with no symptoms or known risk factors. Another way to
determine if a woman has Ovarian Cancer is to take a sample of ovary and
abdominal tissue (Biopsy). The tissue sample is then examined under a
microscope to determine if cancer cells are present.
After menopause, women who are at increased risk of
ovarian cancer or who are experiencing symptoms may choose to have yearly CA_125
blood test. But the CA-125 test does not always detect ovarian
cancer that is present (doctors call this is a "false negative" test result),
CA-125 levels can be elevated because of non-cancerous conditions including
endometriosis, fibroids, pelvic infections,
pregnancy, and menstruation. Other conditions that may raise CA-125 levels
are hepatitis. These factors cause positive readings in
women who do not have ovarian cancer.
Vaginal ultrasound or
computerised tomography (CT scanning) may be used to look at the
ovaries if cancer is suspected. If
the ultrasound of scan does show a tumor, surgery is required to remove the
tumor and rule out cancer. Most of the time, tumors in the ovary are found
to be non-cancerous. Color-flow Doppler, is another type of
ultrasound test that checks the blood flow to the ovaries. An increase in blood
flow to a certain area can be an indication of cancer in that region.
Culdocentesis involves the use of a needle to obtain a
sample of fluid from the vaginal wall and the area surrounding the
ovaries, which can then be analyzed for the presence of cancer cells.
A doctor may use
laparoscopy to diagnose ovarian cancer and
determine the degree to which it has spread. A flexible fibre-optic tube
is inserted into the abdominal cavity by means of a small cut in the skin just
below the navel. A sample of the suspected abnormal tissue, a �biopsy�, may be
taken and sent to the laboratory for microscopic examination to determine
whether this is an ovarian cancer and if so, what sort. Similarly, if fluid has
accumulated in the abdomen, it can be drawn out (aspirated) through a needle and
examined to see whether cancer cells are present. However, it is usually
necessary to perform more extensive surgery (called exploratory laparotomy)
through a larger abdominal incision to establish the diagnosis and full extent
of the cancer.
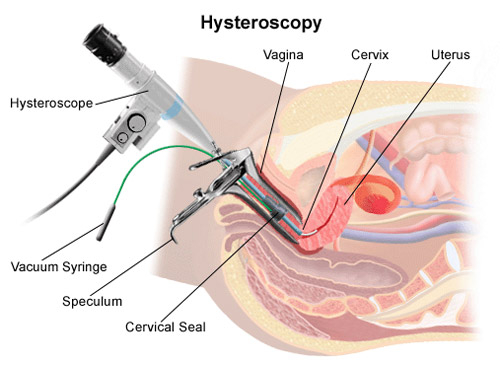
Hysteroscopy- A hysteroscope is an instrument used to see inside the
uterus and fallopian tube. Hysteroscopy is used to diagnose disorders such as
uterine polyps and can be performed under general or local anesthesia
in an outpatient clinic.
Some women at very high risk of ovarian cancer, such as those with more than one
close relative (mother, daughter, aunt, or sister) with the disease, may choose
to have their ovaries removed as a preventive measure. Women who make this
choice usually have completed their childbearing and are nearing menopause.
After surgery, they can replenish and maintain their supply of estrogen by
taking
hormone replacement therapy.
Treatment Options
About 80 to 85 percent of ovarian cancers start in the epithelial cells,
which are cells that cover the surface of the ovaries. Epithelial ovarian
cancer is most common in women over 40. Other types of ovarian cancer,
including those that originate in the egg or the tissue in which the egg grows
inside the ovary, tend to occur in women under 40.
Treatment depends on the type of
cancer and how far it has spread. A woman's age, her general state of
health, and whether or not she has completed her family are all considerations
in the choice of treatment. For example, if a young woman has a tumor in a
very early stage that is confined to one ovary, her doctor may remove only that
ovary to preserve her ability to have children. However, the doctor may
recommend removal of her other ovary and her uterus once she has completed her
childbearing.
Surgical treatment for ovarian
cancer usually consists of removing the ovaries, uterus, cervix, fallopian
tubes, and the
omentum.
Staging is performed by the surgeon (gynecologic oncologist) when the
ovarian cancer is removed.
Ovarian cancer has been linked with 3 hereditary syndromes.
Breast-ovarian cancer syndrome
Hereditary nonpolyposis colorectal cancer syndrome
Site-specific ovarian cancer syndrome
When deciding on a treatment method, doctors consider the
patient's stage of life, general health, and the size and location of any
tumors. In most cases of Ovarian Cancer, a combination of surgery and either
chemotherapy or radiation is used.
|
|
surgical methods are used to treat Ovarian Cancer:
|
Other methods are used to treat Ovarian Cancer:
|
|
|
|
Oophorectomy - This is the removal of one or both of the ovaries
affected by the cancer.
Hysterectomy - This is the removal of the uterus and possibly the
fallopian tubes to remove any tumors that have spread to these organs. This
is usually done in addition to an oophorectomy.
Debulking - This procedure is used for advanced cases. The
ovaries, fallopian tubes and uterus are all removed, as well as any cancer
deposits the surgeon can see, in an effort to remove as many cancer cells as
possible from the body. This procedure is used for advanced cases.
Other treatments:-
 Chemotherapy - Chemotherapy is a systemic, or whole body,
treatment, the goal of which is to kill any remaining cancer cells in the
body and to keep the cancer from spreading to other organs. The drugs are
typically given in cycles of a few days of treatment and then 3-4 weeks of
rest, for a period of weeks or months determined by the oncologist. Drugs
are administered by mouth or injection to kill the cancer cells. The drugs
enter the blood stream and can, therefore, reach areas of the body where the
cancer may have spread. When Ovarian Cancer is confined to the abdomen
(peritoneal carcinomatosis), chemotherapy may be given directly to the
abdominal lining, reducing the number of affected systems and concentrating
the drug's effects in the cancer region. Chemotherapy - Chemotherapy is a systemic, or whole body,
treatment, the goal of which is to kill any remaining cancer cells in the
body and to keep the cancer from spreading to other organs. The drugs are
typically given in cycles of a few days of treatment and then 3-4 weeks of
rest, for a period of weeks or months determined by the oncologist. Drugs
are administered by mouth or injection to kill the cancer cells. The drugs
enter the blood stream and can, therefore, reach areas of the body where the
cancer may have spread. When Ovarian Cancer is confined to the abdomen
(peritoneal carcinomatosis), chemotherapy may be given directly to the
abdominal lining, reducing the number of affected systems and concentrating
the drug's effects in the cancer region.
Radiation - This is the least common treatment for Ovarian Cancer
compared with surgery and chemotherapy. Radiation therapy is the process in
which high-energy x-rays are directed at the affected area in order to kill
cancer cells. Radiation therapy is local, affecting only the area exposed to
the rays. It is typically given five days per week for a period of five or
six weeks.
Biological Therapy - This is a relatively new and for the most
part still experimental method of cancer treatment. It involves using
substances to boost the body's own
immune system responses to kill the
cancer cells. In particular, monoclonal antibodies directed against ovarian
cancer have been developed and are now under study.
-
Infertility - Any surgery that removes the ovaries or
uterus prevents the possibility of becoming pregnant.
- Temporary pain or discomfort due to surgical incisions.
- Early menopause symptoms - Common symptoms are
hot flashes and
vaginal dryness, and are usually treated with hormone replacement therapy. In
the long term, effects of removing the ovaries include
osteoporosis and
increased risks of
coronary artery disease.
- Incontinence - Temporary incontinence or an inability to move the
bowels is sometimes experienced for a short time after surgery.
Click here for Kegel exercise.
The doctor may perform additional
surgery to determine the extent of the cancer's spread beyond the ovaries or, if
it has spread, to take out as much of the cancer as possible. In some
cases, a portion of the intestine must also be removed.
Prevention
Certain lifestyle habits can help to reduce your risk of developing Ovarian
Cancer (as well as other cancers):
- Yearly gynecological exam and pelvic exam
|
|
|
|
|
|
|
|
|
|
|
Find related terms:
Dated 25 February 2014
Related Links
|









